The following interview with Dr. Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization, was conducted by email in April 2025.
LeprosyBulletin (LB): From the perspective of the World Health Organization (WHO), what is the value that each side brings to this partnership?
Dr. Tedros: WHO has brought to this partnership its technical expertise and global coordination capacities, connecting countries and stakeholders around this common goal. During the same period, The Nippon Foundation/Sasakawa Health Foundation (TNF/SHF) has demonstrated its steadfast commitment to leprosy elimination through high-level advocacy and funding support.
The partnership combines policy influence with dedicated resources, creating a unique synergy in the fight against leprosy. It has contributed to reducing the global leprosy burden and continues to pioneer innovative approaches to address the last mile challenges in leprosy elimination.
LB: How would you describe the significance of the partnership’s duration?
Dr. Tedros: The 50-year duration of this partnership is extraordinary in global health and serves as a model for other collaborations. The partnership not only demonstrates the commitment of both organizations but also the complex nature of eliminating leprosy, which requires persistent, multi-generational effort. Leprosy is an ancient disease with medical and social ramifications. Few health-focused collaborations have sustained such longevity while maintaining their original mission. This enduring partnership has enabled sustainability in our efforts to eliminate leprosy despite evolving global health priorities.
LB: What has changed about the fight against leprosy as a result of the partnership?
Dr. Tedros: The main changes in the fight against leprosy that our partnership has contributed to are the reduction in the burden of leprosy and its impact on people affected by the disease. We have moved from an era when leprosy was widely prevalent with limited treatment options to one where elimination of the disease as a public health problem globally was achieved by 2000. This was largely possible due to the support of TNF/SHF, which enabled WHO to introduce multidrug therapy (MDT) globally and scale up its access from 1995 to 1999.
This major success eventually generated a second change: the move towards interruption of transmission and elimination of leprosy. This policy was adopted in 2023 in alignment with the WHO NTD road map 2021−2030.
A third change has been how the partnership has helped broaden the focus of action against leprosy beyond medical interventions. Now, we address key social aspects such as stigma and discrimination, for example, thanks to the establishment of the position of a UN Special Rapporteur focusing on the human rights of persons affected by leprosy and their family members. Our partnership has driven this comprehensive approach, which is embodied in our Global Leprosy Strategy 2021–2030 and its call for zero disease, disability, and discrimination.
LB: The fact that the partnership is ongoing despite over 50 years of efforts reflects the difficulty of eradicating leprosy. What are some of the remaining challenges?
Dr. Tedros: Despite progress, we face significant challenges. Transmission of leprosy continues in endemic hotspots with new cases detected among children, which indicates ongoing community spread. The disease disproportionately affects marginalized populations with limited healthcare access. Longstanding stigma remains deeply entrenched in many societies, hindering health-seeking behaviour, early diagnosis, and treatment. Maintaining political commitment and resources becomes increasingly difficult as the number of cases declines, leading to reduced surveillance and expertise.
LB: How might these challenges be overcome?
Dr. Tedros: Overcoming these challenges requires a multi-faceted approach.
It is important that we strengthen integrated active case-finding strategies in high-burden areas while maintaining passive surveillance capabilities in low-endemic regions. The geographic concentration of cases in specific regions requires tailored approaches rather than one-size-fits-all solutions.
Integrating leprosy services into general healthcare systems ensures sustainability while developing innovative diagnostic tools will help identify cases earlier. We need enhanced community engagement and increased coordination, particularly involving persons affected by leprosy. Education campaigns must continue to address stigma through sharing accurate information. Cross-sector collaboration among health, social welfare, and education sectors can address the broader determinants affecting leprosy.
And critically, political commitment and increased domestic and donor funding are crucial to our last mile efforts in the fight against leprosy.
LB: Please add anything that you would like to say about Yohei Sasakawa’s role as WHO Goodwill Ambassador for Leprosy Elimination and its place in the partnership.
Dr. Tedros: Mr. Sasakawa’s role as WHO Goodwill Ambassador for Leprosy Elimination has been transformative. He has added the much needed human and social dimension to the medical side of the disease. His personal engagement with affected communities around the world has enabled local solutions to the challenges. Mr. Sasakawa has advocated for meaningful participation of people affected by leprosy and for a greater focus on socio-economic aspects. His high-level advocacy with political leaders has kept leprosy on the global health agenda when it might otherwise have been overlooked. The Global Appeal initiatives he has championed have engaged diverse stakeholders from religious leaders to corporate executives in addressing stigma. And his simultaneous role as chairman of TNF has provided a unique bridge between TNF/SHF and WHO that strengthens our institutional partnership through personal commitment and passionate leadership.

LB: We are now at the halfway point of WHO’s Global Leprosy (Hansen’s Disease) Strategy 2021–2030. Considering the impact of the COVID-19 pandemic and other factors, how would you assess the progress toward this goal? What key actions do you believe are necessary to ensure its achievement?
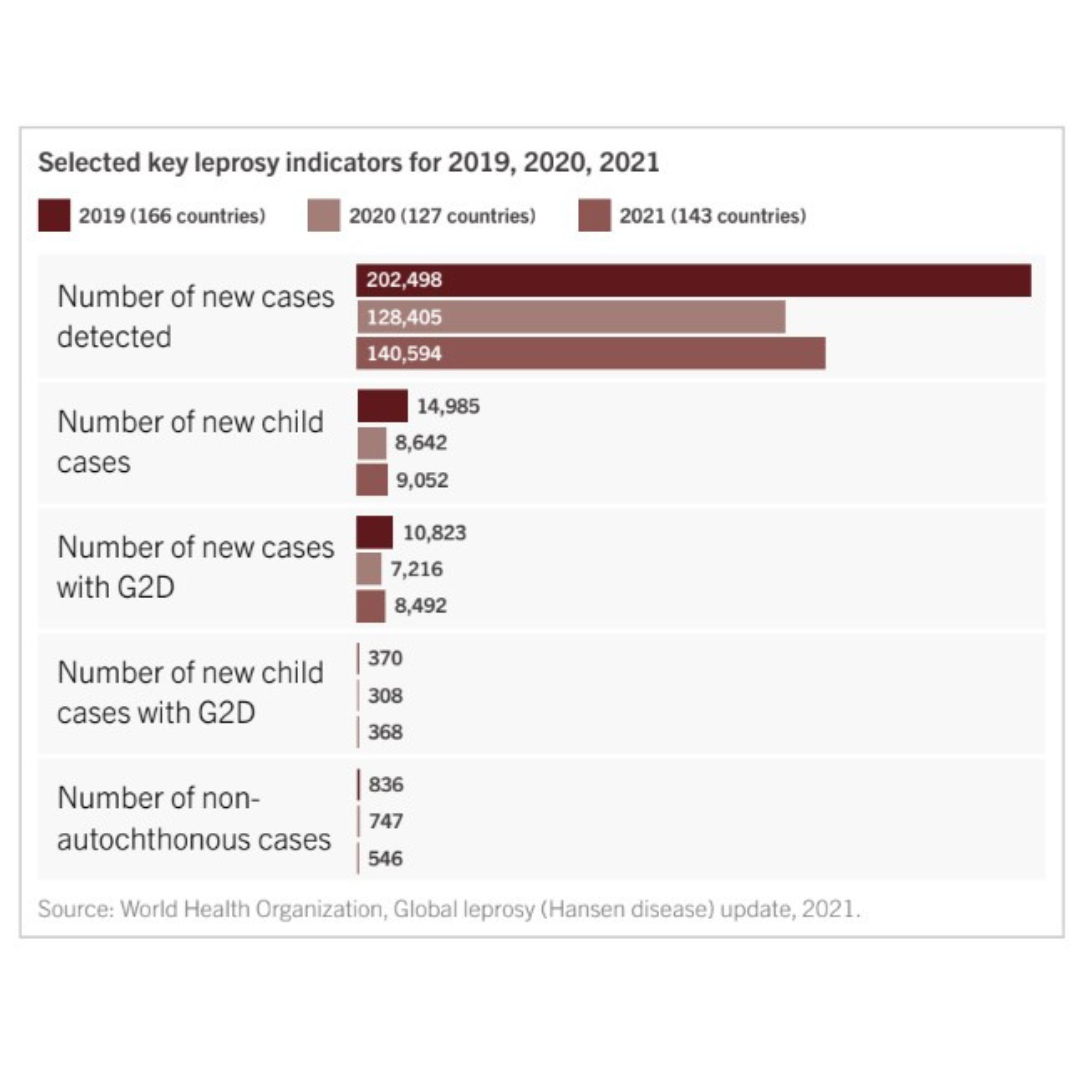
Dr. Tedros: COVID-19 significantly challenged our progress toward the 2030 targets and disrupted essential leprosy services worldwide. Case detection decreased not due to reduced transmission but because of disruption in surveillance and service delivery.
However, the pandemic also accelerated innovations in community-based approaches and digital health solutions that have the potential to strengthen our programs in the long-term. The achievement of elimination of leprosy in Jordan, for example, provides encouragement to other countries.
Moving forward, key actions that we must sustain include rapidly restoring and strengthening disrupted services, accelerating implementation of post-exposure prophylaxis through strengthened contact survey, enhancing community engagement, leveraging digital tools for training and surveillance, and ensuring domestic financing commitments.
Recovery from the pandemic must serve as an opportunity to build back more resilient and integrated program implementation.
LB: How do leprosy elimination efforts fit within the current global public health landscape?
Dr. Tedros: The current global public health landscape presents both challenges and opportunities for leprosy elimination.
Health systems worldwide are simultaneously recovering from the COVID-19 pandemic while confronting multiple threats, including antimicrobial resistance, climate-related health impacts, and non-communicable diseases.
At the same time, the pandemic has heightened awareness about infectious diseases, strengthened laboratory networks, and demonstrated the importance of community health workers – all potentially beneficial for leprosy programs.
New challenges, including geopolitical and financial, are placing increased strains on the budgets of governments, health organizations, and partners globally. Now more than ever, we need to work together, with solidarity and efficiency, to ensure those most in need receive the health services and care they require.
The increased focus on universal health coverage, underpinned by primary health care, creates opportunities to integrate leprosy services with those directed against other neglected tropical diseases, notably through the WHO-recommended skin-NTD approach.
These interventions can also be mainstreamed within the general healthcare system. Similarly, increased attention to health equity and social determinants aligns well with addressing the socioeconomic factors that underlie leprosy transmission and impact.
Partnerships like the 50-year-long collaboration between WHO and TNF/SHF are shining examples of how we can advance health agendas effectively and in a sustained way, and in doing so serve the most vulnerable.