
Ramesh Kumar Choudhary
Manager, Community Health and Development
Nepal Leprosy Trust (NLT)/Lalgadh Leprosy Hospital & Services Centre (LLHSC)
Ramesh pioneered the establishment of LLHSC’s Self-Care Training Centre as well as Nepal’s first Self Help Group (SHG). In his current role, he oversees the hospital’s community programs, including 115 SHGs and various projects for achieving zero leprosy.
When we talk about leprosy, the focus cannot be just within the boundaries of a single country. The disease does not recognize borders, and thus, cooperation and coordination between neighboring countries are essential for effective elimination. Dedicating resources to shared research initiatives and implementing evidence-based strategies across borders can strengthen the drive towards a leprosy-free world.
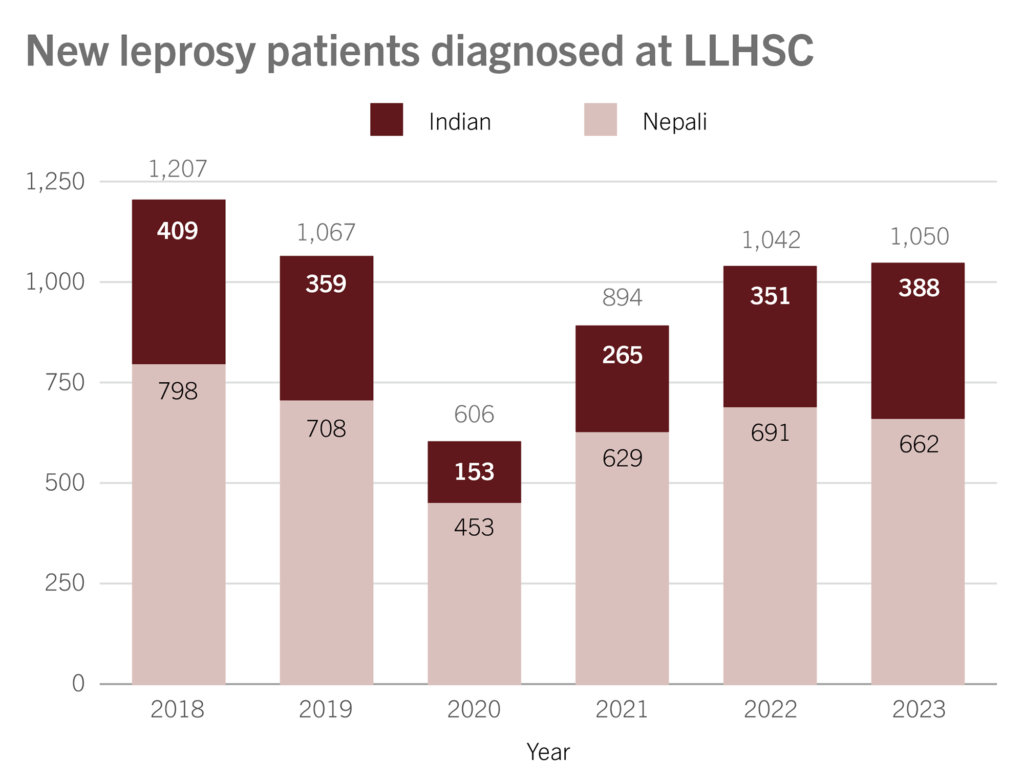
India and Nepal share open borders, allowing their citizens free transit between the two nations. This freedom is utilized for various purposes including seeking medical treatment. Many Indians, in particular, travel to Nepal for leprosy treatment, primarily at the Nepal Leprosy Trust (NLT)/Lalgadh Leprosy Hospital and Services Centre (LLHSC). Roughly 34% of new leprosy patients diagnosed at LLHSC are Indian, and so are 23% of the hospital’s annual in-patient admissions. These patients typically stay for three to six months. All services related to leprosy treatment at the hospital are offered free of charge, irrespective of the patient’s race, caste, gender, or nationality.
Many wonder why NLT/LLHSC is such a favored choice for cross-border care. When queried, Indian patients offered several reasons for preferring LLHSC as their treatment center. These include the provision of high-quality specialized care, a deep cultural understanding and respect, access to excellent facilities and resources, free and easily accessible care, and a comprehensive treatment plan that emphasizes compassionate care.
Complexity arises from the fact that each country has different healthcare systems, cultural norms, and levels of infrastructure. To effectively address leprosy, these differences have to be bridged, and a harmonized approach needs to be adopted. This requires a high level of cooperation, communication, and mutual understanding between the countries involved. Additionally, inclusive and locally tailored strategies that align with each nation’s healthcare framework are vital for the successful elimination of the disease.
One of the major challenges in cross-border leprosy control is the sharing of information. Different countries may have different reporting mechanisms, making it challenging to have a clear understanding of the actual situation. Unified and standardized reporting systems need to be established to ensure that accurate data is available for effective decision-making and resource allocation.
Stigmatization of leprosy-affected individuals is another critical issue that transcends borders. It is essential for neighboring countries to align their efforts in raising awareness and addressing the social stigma associated with leprosy. This requires collaborative education and advocacy programs that can have a cross-border impact.
Developing a unified strategy for cross-border leprosy control is pivotal. This involves aligning treatment protocols, sharing best practices, and coordinating efforts in contact tracing and surveillance. By working together, neighboring countries can ensure that there are no gaps in the control and elimination of leprosy within their shared regions.
In conclusion, to effectively combat leprosy, countries must work together, transcending boundaries and collaborating for the greater good. Addressing cross-border issues will not only help in the elimination of leprosy but also set a precedent for global health cooperation and solidarity.







-12.png)